Overview
Gram-positive cocci are a cornerstone of USMLE Step 1 microbiology. You'll encounter them frequently in clinical vignettes, so understanding their key characteristics, common infections, and distinguishing features is paramount. This section will equip you with the knowledge to confidently identify and differentiate these important pathogens, focusing on what the USMLE loves to test.
Core Concepts
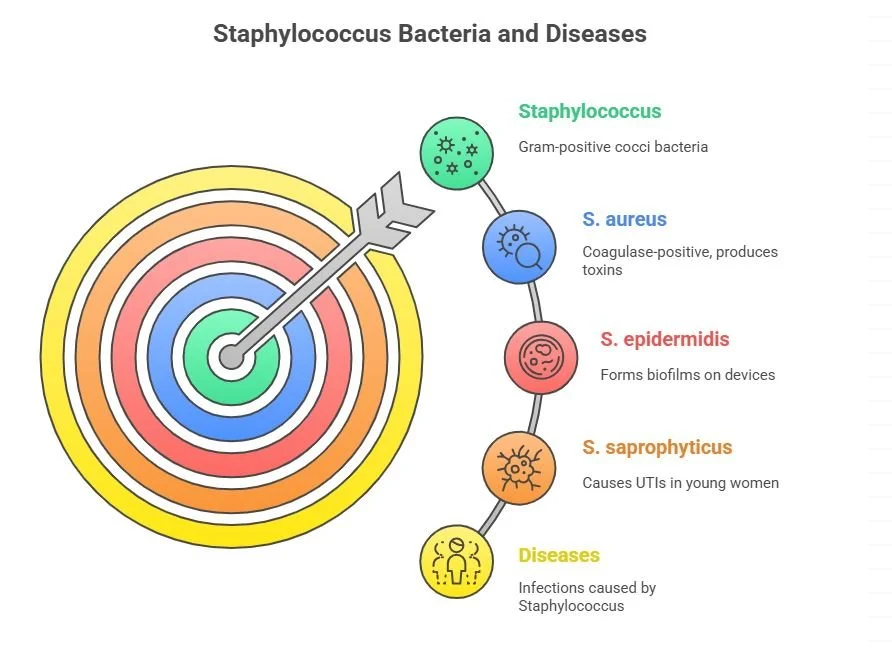
Staphylococcus
Classification & Morphology: Gram-positive cocci in clusters (like grapes). Catalase-positive (differentiates from Streptococcus). Staphylococcus aureus is coagulase-positive (forms clots), while Staphylococcus epidermidis and Staphylococcus saprophyticus are coagulase-negative.
Physiology & Virulence Factors:
S. aureus: Produces a wide array of virulence factors, including Protein A (binds Fc region of IgG, preventing opsonization and phagocytosis), coagulase, hemolysins, enterotoxins (food poisoning), toxic shock syndrome toxin (TSST-1, a superantigen), and exfoliative toxins (scalded skin syndrome).
S. epidermidis: Forms biofilms on prosthetic devices (e.g., catheters, artificial heart valves), making it resistant to antibiotics and host defenses.
S. saprophyticus: Adheres to uroepithelial cells, a common cause of UTIs in sexually active young women.
Major Diseases:
S. aureus: Skin infections (folliculitis, furuncles, carbuncles, impetigo), cellulitis, osteomyelitis, septic arthritis, endocarditis (especially in IV drug users affecting the tricuspid valve), toxic shock syndrome, food poisoning (preformed toxin), scalded skin syndrome.
S. epidermidis: Prosthetic device infections (e.g., prosthetic heart valves, joint replacements, catheters), endocarditis (on native or prosthetic valves).
S. saprophyticus: Urinary tract infections (UTIs), particularly in young, sexually active women.
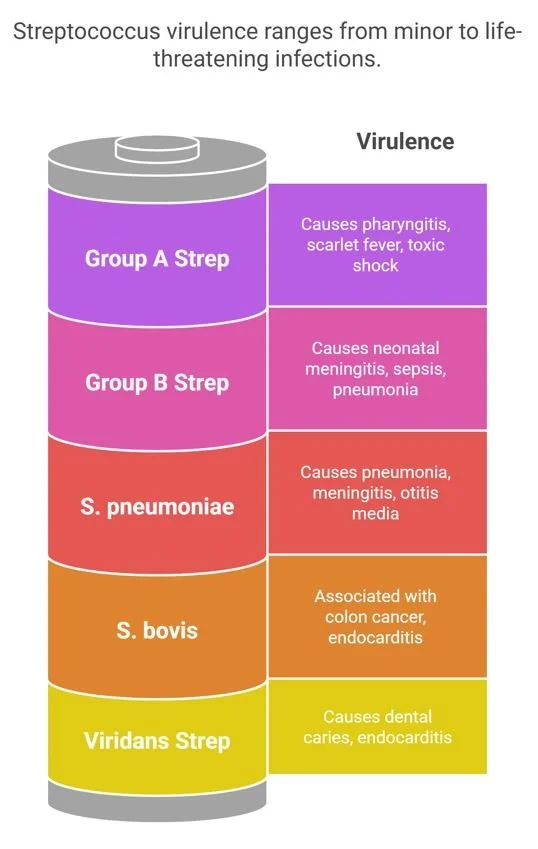
Streptococcus
Classification & Morphology: Gram-positive cocci in chains. Catalase-negative (differentiates from Staphylococcus). Classified by hemolysis on blood agar (alpha, beta, gamma) and Lancefield grouping (based on carbohydrate antigens in cell wall).
Physiology & Virulence Factors:
Group A Strep (S. pyogenes): M protein (antiphagocytic, mimics host proteins), streptolysin O (lyses RBCs, immunogenic), streptokinase (fibrinolysis), hyaluronidase (breaks down connective tissue), pyrogenic exotoxins (scarlet fever, toxic shock-like syndrome).
Group B Strep (S. agalactiae): Polysaccharide capsule (antiphagocytic), CAMP factor (enhances hemolysis of S. aureus).
S. pneumoniae: Polysaccharide capsule (major virulence factor, antiphagocytic), IgA protease.
Viridans Strep (S. mutans, S. sanguinis): Produce dextrans from sucrose, allowing adherence to heart valves (endocarditis) and tooth enamel (dental caries).
Major Diseases:
Group A Strep (S. pyogenes): Pharyngitis (strep throat), scarlet fever, impetigo, cellulitis, erysipelas, necrotizing fasciitis, streptococcal toxic shock syndrome. Post-streptococcal complications: Rheumatic fever (Type II hypersensitivity, affects heart valves, joints, brain) and Post-streptococcal glomerulonephritis (Type III hypersensitivity, periorbital edema, dark urine).
Group B Strep (S. agalactiae): Neonatal meningitis, sepsis, pneumonia (transmitted vertically from mother to infant during birth). Also causes UTIs in pregnant women.
S. pneumoniae: Most common cause of lobar pneumonia, otitis media, meningitis, and sinusitis (MOPS). Encapsulated.
Viridans Strep: Subacute bacterial endocarditis (damaged heart valves), dental caries.
S. bovis (now S. gallolyticus): Associated with colon cancer and endocarditis.
Mnemonic and Memory Aids
Staphylococcus vs. Streptococcus:
Catalase Test: Staph are Catalase-positive (they have a CAT). Strep are No Catalase (no cat).
Coagulase Test (for Staph): S. aureus is Coag-positive (it's the gold standard, like golden coagulation). Coagulase-negative Staph (CoNS) are S. epidermidis and S. saprophyticus.
S. aureus Virulence Factors:
S. aureus Virulence Factors (mnemonic: "STAPH AUREUS Toxins")
* Scalded skin syndrome (exfoliative toxin)
* Toxic shock syndrome (TSST-1 superantigen)
* Acute endocarditis, Arthritis, Abscesses
* Pneumonia * Hospital-acquired infections
* Aureus (the name itself)
* Urinary tract infections (less common, but can occur)
* Really bad food poisoning (enterotoxin)
* Erysipelas (can be caused by S. aureus too, though more commonly Strep)
* Unique virulence factors: Protein A (binds Fc of IgG), Coagulase
* Skin infections (impetigo, cellulitis, furuncles, carbuncles)
Streptococcus Pyogenes (Group A Strep) Virulence Factors (mnemonic: "STREP THROAT")
Streptolysin O (lyses RBCs, immunogenic)
Toxic shock-like syndrome (pyrogenic exotoxin)
Rheumatic fever (M protein)
Erysipelas
Pyogenic exotoxin (scarlet fever)
Throat infection (pharyngitis)
Hyaluronidase
RNAse (less high-yield)
Outstanding complications: Post-streptococcal Glomerulonephritis (Type III HSR)
Antiphagocytic: M protein
Tissue damage: Streptokinase (fibrinolysis)
Streptococcus Pneumoniae (MOPS):
Meningitis
Otitis media
Pneumonia
Sinusitis
Key Virulence Factor: Polysaccharide Capsule (major target for vaccines).
Integration with Other Subjects
Immunology:
S. aureus Protein A: This virulence factor is a classic example of immune evasion. By binding the Fc portion of IgG, it prevents opsonization and phagocytosis. Recall from your immunology studies that the Fc region is typically recognized by phagocytes (like macrophages and neutrophils) and activates complement. Protein A essentially cloaks the bacterium from these immune defenses.
S. pyogenes M Protein: This protein is highly antiphagocytic and mimics host proteins, contributing to the autoimmune response seen in Rheumatic Fever. Remember that molecular mimicry is a key concept in autoimmune diseases.
Superantigens (TSST-1 from S. aureus, Pyrogenic Exotoxins from S. pyogenes): These toxins bypass normal antigen presentation by directly cross-linking the T-cell receptor (TCR) beta chain to the MHC class II molecule on antigen-presenting cells (APCs). This leads to massive, non-specific T-cell activation and a cytokine storm, causing systemic symptoms like fever, rash, and shock. This is a critical concept to review from your immunology lectures on T-cell activation.
Post-streptococcal Glomerulonephritis (PSGN): A Type III Hypersensitivity reaction. Antigen-antibody complexes (formed between streptococcal antigens and host antibodies) deposit in the glomeruli, activating complement and causing inflammation. This links directly to your understanding of hypersensitivity reactions.
Rheumatic Fever: A Type II Hypersensitivity reaction (molecular mimicry). Antibodies against streptococcal M protein cross-react with host tissues (heart, joints, brain), leading to inflammation and damage. This is another direct link to hypersensitivity types.
Pathology:
S. aureus Endocarditis: Often causes acute endocarditis, particularly on previously healthy valves, and is common in IV drug users (affecting the tricuspid valve). This contrasts with Viridans Strep, which typically causes subacute endocarditis on previously damaged valves.
Necrotizing Fasciitis: A rapidly progressive, life-threatening infection often caused by S. pyogenes (Group A Strep), leading to extensive tissue destruction. Pathology will emphasize the rapid spread along fascial planes and the severe inflammatory response.
Osteomyelitis and Septic Arthritis: S. aureus is the most common cause of both, especially in children. Understanding the inflammatory changes in bone and joints is key.
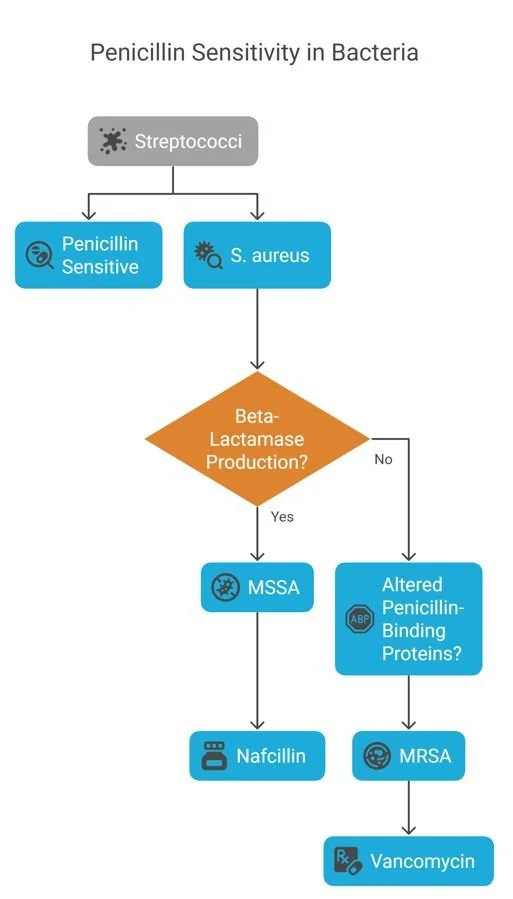
Pharmacology:
Penicillin Sensitivity: Most streptococci are highly sensitive to penicillin. However, S. aureus is often penicillin-resistant due to beta-lactamase production (methicillin-sensitive S. aureus - MSSA) or altered penicillin-binding proteins (methicillin-resistant S. aureus - MRSA). This highlights the importance of understanding antibiotic resistance mechanisms and choosing appropriate antibiotics (e.g., nafcillin for MSSA, vancomycin for MRSA).
Vancomycin: The drug of choice for MRSA and serious CoNS infections. Remember its mechanism of action (inhibits cell wall synthesis by binding D-Ala-D-Ala) and potential side effects (red man syndrome, nephrotoxicity, ototoxicity).
Biochemistry:
S. mutans (Viridans Strep): Produces dextrans from sucrose, which are glucose polymers that allow the bacteria to adhere to tooth enamel and heart valves. This connects to carbohydrate metabolism and bacterial adhesion mechanisms.
Clinical Correlation
Vignette 1: A 23-year-old medical student presents to the emergency department with a 2-day history of fever, malaise, and a painful, swollen right knee. He admits to occasional intravenous drug use. Physical examination reveals a warm, erythematous, and tender right knee with limited range of motion. Arthrocentesis yields purulent synovial fluid. Gram stain of the fluid shows Gram-positive cocci in clusters. Which of the following is the most likely causative organism?
Explanation: The key buzzwords here are
"intravenous drug use," "painful, swollen right knee" (septic arthritis), and "Gram-positive cocci in clusters." This constellation strongly points to Staphylococcus aureus, which is a common cause of septic arthritis, especially in IV drug users where it often affects large joints like the knee. The Gram stain finding of cocci in clusters further confirms the staphylococcal morphology. The USMLE loves to test S. aureus in the context of IV drug use and associated infections like endocarditis (tricuspid valve) and septic arthritis.
Vignette 2: A 3-day-old male neonate is brought to the clinic by his mother due to poor feeding, lethargy, and a rectal temperature of 101.5°F (38.6°C). The mother had no prenatal care. Physical examination reveals a listless infant with a bulging fontanelle. Lumbar puncture is performed, and CSF analysis shows elevated white blood cell count with neutrophil predominance, decreased glucose, and elevated protein. Gram stain of the CSF reveals Gram-positive cocci in chains. Which of the following is the most likely pathogen?
Explanation: The critical information here is the "3-day-old male neonate," "poor feeding, lethargy, bulging fontanelle" (signs of meningitis), and "Gram-positive cocci in chains" in the CSF. This clinical picture is highly suggestive of neonatal meningitis caused by Streptococcus agalactiae (Group B Strep). GBS is a leading cause of sepsis and meningitis in neonates, typically acquired vertically during birth. The Gram stain showing cocci in chains differentiates it from Staphylococcus. The USMLE frequently tests GBS in the context of neonatal infections and the importance of maternal screening and prophylaxis.
High-Yield Exam Tips
Catalase Test is Key: Always use the catalase test to differentiate between Staphylococcus (positive) and Streptococcus (negative) first. This is a fundamental step in Gram-positive cocci identification.
Coagulase Test for Staph: Once you know it's Staphylococcus, the coagulase test is crucial. S. aureus is coagulase-positive (the bad one!), while S. epidermidis and S. saprophyticus are coagulase-negative. This distinction guides diagnosis and treatment.
S. aureus = IV Drug Use & Abscesses: Think S. aureus for infections in IV drug users (tricuspid endocarditis, septic arthritis) and for abscess formation (skin, bone, organ).
S. pyogenes = Post-Strep Complications: Remember the two major non-suppurative complications of S. pyogenes infections: Rheumatic Fever (affects heart, joints, brain; Type II HSR) and Post-streptococcal Glomerulonephritis (affects kidneys; Type III HSR). Know the differences in their latency and affected organs.
S. pneumoniae = MOPS: This encapsulated bacterium is the most common cause of Meningitis, Otitis media, Pneumonia, and Sinusitis. Vaccination targets its polysaccharide capsule.
Mini Quiz
Question 1: A 65-year-old man with a history of poorly controlled diabetes mellitus presents with a painful, red, swollen left foot. He denies any recent trauma. Physical examination reveals a large, fluctuant abscess on the plantar aspect of his foot. Gram stain of pus from the abscess shows Gram-positive cocci in clusters. Culture grows an organism that is catalase-positive and coagulase-positive. Which of the following is the most appropriate initial antibiotic therapy?
A) Penicillin G B) Vancomycin C) Ampicillin D) Ceftriaxone E) Doxycycline
Explanation: The patient presents with a diabetic foot ulcer complicated by an abscess, and the Gram stain shows Gram-positive cocci in clusters that are catalase-positive and coagulase-positive. This confirms the causative agent as Staphylococcus aureus. Given the high prevalence of MRSA (Methicillin-Resistant Staphylococcus aureus) in skin and soft tissue infections, especially in patients with risk factors like diabetes, empiric coverage for MRSA is crucial. Vancomycin (B) is the drug of choice for suspected or confirmed MRSA infections. Penicillin G (A) and Ampicillin (C) would not cover MRSA. Ceftriaxone (D) is a third-generation cephalosporin that also lacks reliable MRSA coverage. Doxycycline (E) can be used for some MRSA strains but is not typically the first-line empiric choice for a severe abscess in this setting.
Question 2: A 7-year-old boy is diagnosed with pharyngitis. Two weeks later, he develops migratory polyarthritis, carditis, and subcutaneous nodules. A rapid streptococcal antigen test was positive during his pharyngitis episode. Which of the following virulence factors is most likely responsible for the subsequent development of his current condition?
A) Protein A B) M protein C) Polysaccharide capsule D) Streptolysin O E) Exfoliative toxin
Explanation: The clinical presentation of pharyngitis followed by migratory polyarthritis, carditis, and subcutaneous nodules is classic for Rheumatic Fever, a non-suppurative complication of Streptococcus pyogenes (Group A Strep) infection. The M protein (B) is the primary virulence factor responsible for Rheumatic Fever due to molecular mimicry, where antibodies produced against the M protein cross-react with host tissues. Protein A (A) is a virulence factor of Staphylococcus aureus. The polysaccharide capsule (C) is a major virulence factor for Streptococcus pneumoniae and Streptococcus agalactiae. Streptolysin O (D) is a hemolysin produced by S. pyogenes but is not directly responsible for Rheumatic Fever (though antibodies to it are used for diagnosis). Exfoliative toxin (E) is produced by Staphylococcus aureus and causes scalded skin syndrome.